At night I can’t sleep
In the morning I can’t wake up
We sometimes joke about someone we know, husband, partner, and children about how loud they snore. While snoring may be harmless as in primary or benign snoring, the question is do we keep joking about it or take it more seriously?
Recent study conducted by Dr Robert Deeb* indicated that snoring has its hidden dangers causing thickening of the walls of the carotid arteries.
“Snoring is more than a bedtime annoyance and it shouldn’t be ignored. Patients need to seek treatment in the same way they would if they had sleep apnea, high blood pressure or other risk factors for cardiovascular disease,” says lead study author Robert Deeb, M.D., with the Department of Otolaryngology-Head & Neck Surgery at Henry Ford.

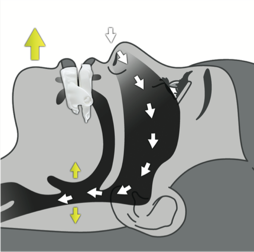
Worse, snoring may be indicative of something much worse, such as OSA (Obstructive Apnoea). If you have OSA that means you stop breathing (airway is either partially or totally blocked) for more than 10 seconds while you are asleep.
Red flags:
- Loud snoring with chortling and choking sounds
- When waking up feeling unrefreshed with a dry mouth
- Frequently falling asleep during the day, such as when reading a book, watching TV, and driving!
- Overweight High blood pressure
If you have any of the above, it is always a good idea to see your GP and to have a good diet and regular exercises. In addition to see your GP, it is also important to see your dentist. Most people are not aware of the increasing role of dentists in sleep management.
Signs and symptoms dentists see in people’s mouth
- Crowded teeth. The jaws are underdeveloped, there is less space for the tongue, consequently, the tongue is pushed back, narrowing the airway.
Receded chin. For the same reason as above, the lower jaw is forced back to fit against the upper jaw. The tongue is taken for a ride, narrowing the airway. - Torus mandibularis. As a dentist I see this hard bony structure in the mouth on a daily basis. These are bony overgrowths inside the lower jaw, usually present as a pair, one on either side of the tongue. Virtually all patients who possess these tori tend to exhibit grinding and clenching habits, especially at night time.
- Gagging. This occurs at the dental chair when the dentist inserts a dental instrument in the mouth, contacting the tongue. Gagging also commonly occur during impression and X ray taking. In all of the cases above, the tongue tends to overreact to any external stimuli, with an almost violent response to push any foreign objects out of the mouth. Gaggers are usually chronic mouth breathers, they tend to breathe through the mouth more than the nose, thus rendering the mouth as a primary breathing apparatus. Any threats to the airway will command an exaggerated response from the tongue and the throat. This is a primal survival instinct, if airway is obstructed, we die. This doesn’t happen with nasal breathers, as the mouth is only a secondary breathing apparatus. The mouth is designed for eating and talking, it is not designed for breathing. I also observe that many of these patients are overweight, although being overweight is not an essential criteria to have OSA.
- Patients falling asleep at the dental chair. I used to think when a patient falls asleep at my chair that I was such a gentle dentist with this incredible ability to relax my patients. Having learned more about sleep and breathing disorders (SDB), unfortunately for my ego this is not quite the case. Patients fall asleep anywhere because they did not have a good quality sleep the night before, and the night before…
Importance Of Sleep
Sleep is absolutely essential for a healthy person to thrive. During the day when we are awake the body needs to move, to keep our vital organs to function optimally. The fight and flight (sympathetic) system is activated in response to the day to day activities. At night time, we sleep, and our rest and digest (parasympathetic) system must over ride the sympathetic system to ensure that all our cells heal and regenerate to prepare the body for the rigors of the following day. But if the body is not allowed to rest without having adequate amounts of quantity AND quality of sleep, it will not function to its optimal level, and it is not surprising that people with poor sleep suffer form chronic diseases such as heart conditions, strokes and diabetes. One of the main causes of poor sleep is airway obstruction.
During sleep, almost all muscles of the body are relaxed and loose. The tongue in particular tends to fall back towards the back of the throat, narrowing the airway. Airway obstruction typically occurs more frequently during the REM cycle of sleep, when all muscles (except for the eyes and the abdomen) are paralysed. In severe cases, the airway can be completely blocked off by the tongue, worsened when sleeping on the back due to gravity. Some patients literally stop breathing (can be more than 30 seconds each time) and forcibly woken up with chortling and choking sounds gasping for air. Here, the sympathetic system trumps the parasympathetic system, rendering increased levels of stress hormones, such as adrenaline and cortisol, which in turn suppresses the immune system.
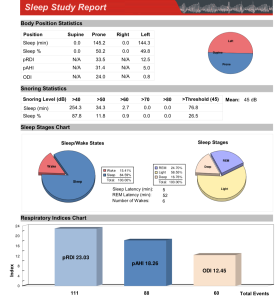
Sleep Study
If there is a suspicion of a sleep disorder, a sleep study is strongly recommended. The study will reveal several indicators:
AHI (Apnoea/Hypopnoea Index) – this measures the number of episodes the breathing is stopped for more than 10 seconds
RDI (Respiratory Disruption Index) – it measures the the number of episodes sleep is interrupted, associated with arousals)
ODI (Oxygen Desaturation Index) – it measures the number of episodes the Oxygen level falls more than 4%.
A sleep study also routinely measures pulse, loudness of snoring (in Decibels), proportions of Deep and REM sleeps and body positions. The gold standard is to conduct a PSG (Polysomnograph) sleep study at a Sleep Clinic. Several Sleep clinics now offer Medicare bulk billing without the out of pocket expenses. One of the disadvantages of the PSG is that the study is conducted away from the home environment. Alternatively, the WatchPat monitor (see picture below) is a more convenient portable sleep unit, where you can sleep in your own bed, and the unit is a lot less invasive than the standard PSG monitor. The disadvantage is that Medicare or private insurance does not cover the cost of the unit.
 At my practices I now routinely use the WatchPat ($250.00) as a screening tool.
At my practices I now routinely use the WatchPat ($250.00) as a screening tool.
A diagnosis of OSA is made when the AHI is greater than 5. Mild OSA is between 5 and 15, moderate OSA is between 15 and 30, severe OSA is more than 30.
What After Sleep Study?
If the diagnosis is severe OSA, ie the AHI Index is greater than 30, it would be wise to see a Sleep Physician who most likely would recommend a CPAP machine.
WatchPat
 Mild and moderate OSA sufferers can be comfortably treated with a sleep appliance. The main objective of the appliance is to advance and hold the lower jaw forward, keeping the airway open. There are numerous sleep appliances, including those to treat snoring, that can be purchased on the internet. They can be as cheap as $50.00. Buyers beware, some of these appliances can make the situation worse. The best sleep appliance must be comfortable to wear, with minimal amount of bulk, but maintaining strength. It must also be adjustable allowing it to position the lower jaw in the optimum position.
Mild and moderate OSA sufferers can be comfortably treated with a sleep appliance. The main objective of the appliance is to advance and hold the lower jaw forward, keeping the airway open. There are numerous sleep appliances, including those to treat snoring, that can be purchased on the internet. They can be as cheap as $50.00. Buyers beware, some of these appliances can make the situation worse. The best sleep appliance must be comfortable to wear, with minimal amount of bulk, but maintaining strength. It must also be adjustable allowing it to position the lower jaw in the optimum position.
One such appliance is Panthera, which I use routinely at my practice.
Panthera
 Procedure in wearing a sleep appliance
Procedure in wearing a sleep appliance
- Conduct a sleep study (baseline report)
- Wear the Panthera sleep appliance for 2-4 weeks.
- Conduct a second sleep study (follow up report after wearing the appliance).
- The appliance will then be adjusted according to the follow up report from the second study. The appliance will be further adjusted until the ‘sweet spot’ is found, that is when all 3 indicators (AHI, RDI and ODI) are below 5.
As a bonus, the manufacturer claims 95% success rate in reducing snoring. Management of sleep/breathing disorders is not simple, it requires careful planning with close cooperation between
Before and After Sleep Study Reports
|
nitial (baseline) sleep study report
Before treatment:
|
Sleep report 4 months after wearing Panthera
After treatment:
|
Summary
Snoring must not be ignored as it may reveal a far more serious underlying health problem. An approved sleep appliance in the hands of a qualified dentist will provide an invaluable treatment in sleep medicine. The appliance can be adjusted to promote optimum sleep hygiene. The adjustments must be made based on objective data obtained from the sleep studies.
Reference
*Henry Ford Health System. “Don’t ignore the snore: Snoring may be early sign of future health risks.” ScienceDaily. ScienceDaily, 24 January 2013. www.sciencedaily.com/releases/2013/01/130124122741.htm